My name is Ming Huang, an assistant professor in Computational Systems Biology Laboratory. After I graduated from the University of Aizu in 2012, I was a postdoc fellow of NAIST for three and a half years. In this essay, I would like to share some of my thinking related to my study filed with you all.
The technologies featured with ‘wearable’, ‘nonconscious’ characteristics have been being popular in the past few years. It is one of the major domains that will output tremendous amount of data about personal health, and it is a major part of health informatics. Health informatics also involves the information of personal medical data in the form of electronic medical records (EMRs). On the other side, the blueprint of life−the genomic information, is the fundamental factor that bears great amount of information about the origin of life. These two domains together, with the personal health being its focus, are supposed to be able to describe how people adjust themselves to adapt to the external environment and stimulation. I had a great opportunity to engage in studies of the health informatics and now extend into bioinformatics in Computational Systems Biology Lab. Therefore, I would like to introduce parts of ours studies on health informatics and then my opinions about integrating the health informatics with bioinformatics for a novel understanding about human health.
Health informatics involves the aspects of acquiring, storing, retrieving and using of the healthcare information and I would only talk about the acquiring and using aspects here.
Acquiring healthcare information
There are two major sources of the healthcare information, one is generated in hospital describing personal medical, treatment histories and biopsy results. This information will become more useful and versatile when it is organized in the form of EMR. The other major source is the daily healthcare devices, which present in various forms such as wrist band, finger rings or even chair and bed. These real-time biomedical or health monitors allow for the characterization of intra-individual physiological variation and the inter-individual impact of circadian fluctuations on physiological measures. Further, they provide the clinicians and scientists with temporal resolutions to examine physiology and therefore a new way to study human diseases. Two studies about how to acquire vital signs (heart rate, respiration rate, blood pressure and temperature) by noninvasive/wearable modalities will be shown below.
Wearable deep body thermometer
Deep body temperature (DBT) is the temperature of the natural cavities, such as abdomen and thorax. It is conventionally measured by the invasive methods using catheter inserted into rectum or esophagus. Alternative measurements inside the mouth or ear canal are also adopted for intermittent measurement. However, the fluctuation of DBT bears more information in its temporal variation, e.g., the circadian rhythm, therefore a wearable DBT thermometer being able to keep track of the DBT will provide more information about the fluctuation of physiology.
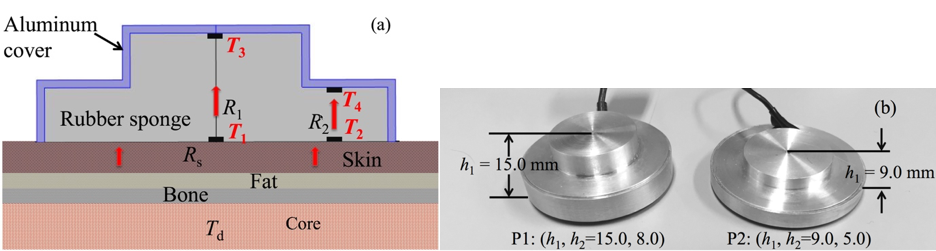
To develop a wearable Deep Body thermometer, the dual heat-flux method (DHFM) has been used. It calculates the DBT based on the heat flux inside a probe as shown in Fig. 1 (a). The double heat paths inside the probe shown by red arrows enable calculation of the DBT by the embedded temperature sensors. A substrate material with four embedded temperature sensors form the core of the probe. The substrate material has physical properties similar to those of skin and, when attached to the skin, most of the heat flow from the core body due to the difference between the DBT and the skin temperature will flow into the substrate material. After the initial period for heat equilibrium establishment, the DBT can be calculated with the four embedded temperature sensors. With this wearable modality, this DBT thermometer should be able to answer to the needs of realistic applications such as the prevention of heat stroke and the estimation/adjustment of disorder of circadian rhythm.
Validations of device performance is on-going, what we can show is the studies about its accuracy and use in circadian rhythm estimation. We carried out a fast-changing CBT measurement (55 min, 12 subjects) inside a thermostatic chamber. When compared with a reference, the CoreTemp CM-210 by Terumo, the experiment shows 0.07 °C average difference of the prototype.
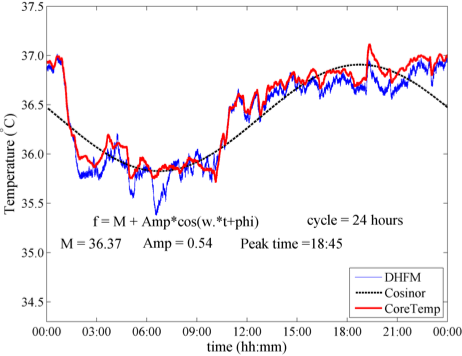
As for the circadian rhythm estimation, we performed long-term monitoring of CBT (24 h, 6 subjects), whose result shows no significant difference in parameters for the inference of circadian rhythm. A whole-length record of a subject is shown in Fig.2. It shows a very standard fluctuation of core body temperature that subjects to circadian rhythm. Red line denotes the measurement by the reference and blue line denotes the measurement by the DBT thermometer prototype. The cosine fitting curve was generated with the measurement by DHFM-based probe and shown in the broken black line.
[1] M. Huang et al, “A Wearable thermometry for core body temperature measurement and Its Experimental Verification,” IEEE J. Biomed. Health Inform., 2016, Feb. for Epub
Non-occlusive blood pressure measurement
Blood pressure (BP) is another important physiological parameter that can’t be measured in an easy way. The standard occlusive method is for intermittent measurement and needs an inflatable cuff to occlude the arterial supply to the distal limb, so as to estimate the systolic and diastolic BP. But actually, the temporal variation of the BP provides important information about the cardiovascular physiology. A non-occlusive way, the so-called cuffless method, that can measure BP continuously can fully retain the temporal information.
we therefore tried to develop an unobtrusive cuffless BP monitoring system. This system is based on pulse transit time (PTT), which is defined as the time taken for an artery pulse to travel between two arterial sites, to facilitate long-term home BP monitoring.
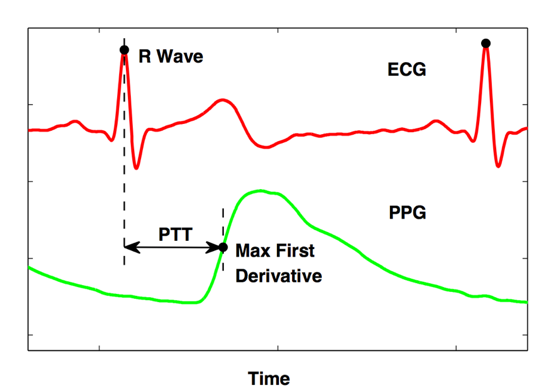
PTT can be simplified as the time delay between the peak of the R wave in the electrocardiogram (ECG) and the corresponding point in photoplethysmogram (PPG) signals as shown in Fig. 3.
Theoretically, we can consider that the pulse wave velocity (PWV), the velocity at which the blood travels along the vessel, is proportional to the square root of elastic module (EM) of the vessel. Further, the EM of the vessel increases exponentially with BP. Therefore, we may be able to estimate the BP based on the PWV.
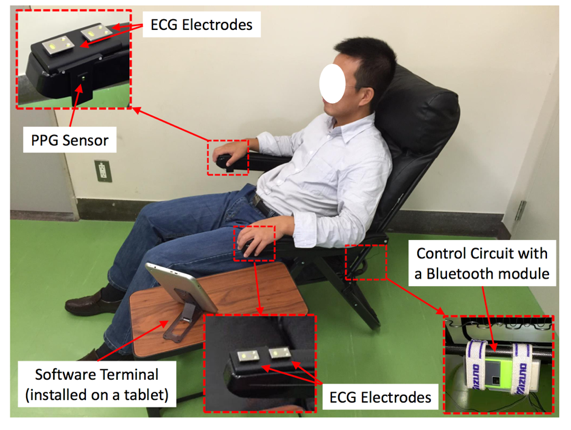
The proposed system mainly includes an ECG module, a PPG module and the control unit and was implemented into a chair as shown in Fig. 4.
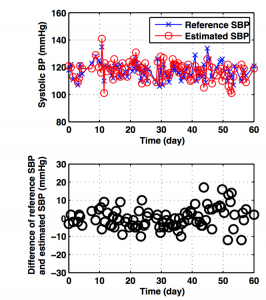
This method can estimate the BP fluctuation around the basic point, and therefore, needs calibration periodically. The duration, the longer the better, is closely related to the way of the calibration, such as the user should calibrate under peaceful condition, the gesture should be consistent in both calibration and measurement. Our system takes advantage from the setup in the form of the chair and we carried out the experiment to monitor the BP for 60 days with only one calibration at the very first day. Fig. 5 shows the result in whole length, where most differences are within the range of ± 10 mmHg for the former 42 days. Data from more subjects should be collected, but it shows the possibility that this system is capable to provide a stable BP measurement within one month.
[2] Z. Tang et al, “A Chair-based Unobtrusive Cuffless Blood Pressure Monitoring System Based on Pulse Transit Time.,” IEEE J. Biomed. Health Inform., Accepted for publication Oct. 2016.
Using the healthcare information
With the great amount of data, we could do more than just plotting the raw data, in other words, using this data for modeling and prediction for the personal physiology will make full use of the data. We should also bear in mind that the wearable and nonconscious devices are vulnerable to external influences, an appropriate way to remove the noisy signal so as to fully reveal its physiological significance initially, the so-called pre-processing, would be indispensable for the successive analyses.
As an example, a widely-acknowledged procedure for the pre-processing of electrocardiograph is the removal of high frequency noise and baseline wandering by corresponding filters. A low-pass finite impulse response (FIR) filter with its cut-off frequency around 40 Hz is suitable to remove high frequency noise, while a high-pass FIR filter with its cut-off frequency around 0.8 Hz is appropriate to remove the baseline wandering. For the signal acquired by wearable modality of relatively low quality, techniques such as biorthogonal wavelets would have a better performance.
With carefully processed healthcare information, we will be able to develop more sophisticated and elegant models for individual normal physiology, and enable identification of subtle or event-induced changes toward pathophysiology early in the course of disease progression.
Integration of health informatics with bioinformatics
Translating the finding from data-intensive biological studies to effective therapies, diagnostic acids and clinical interventions is common nowadays. Temporal profiling of a subject over 14 days using biological (genomics, proteomics, metabolomics and transcriptomics) and clinical phenotypes have revealed how longitudinal measurements of multiscale biological data showed the dynamics of biological pathway during illness and wellness [3].
This kind of works can be attributed to the relatively new domain of translational bioinformatics. Translational Bioinformatics is the development of storage, analytic, and interpretive methods to optimize the transformation of increasingly voluminous biomedical data, and genomic data, into proactive, predictive, preventive, and participatory health.
In the context of translational bioinformatics, individualized risk model being able to discern innocuous deviation from the average population from pathologic changes is of paramount importance.
It certainly is a fast-evolving and exciting domain, for there are a broad space to be explored. For example, how to choose the data streams and determine their clinical significances; how to embed these streams into EHR so as to integrate with biomedical data should be addressed before it can exert great impact on human health.
This domain will finally compose the intact image about personal health. And I do believe it will change the conventional clinical thinking about health in a way.
[3] R. Chen, et al. “Personal omics profiling reveals dynamic molecular and medical phenotypes.” Cell 148.6 (2012): 1293-1307.
